Background
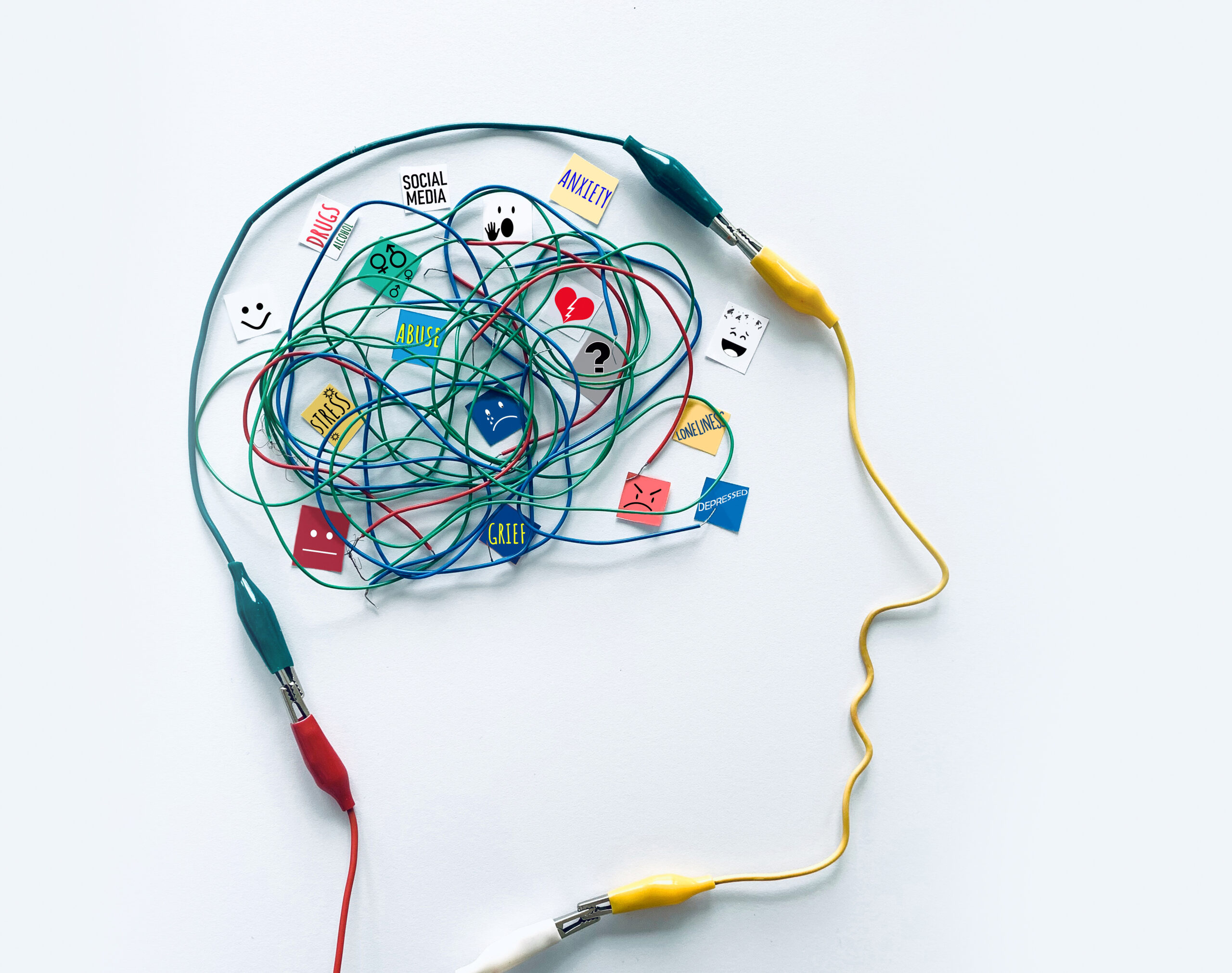
A patient attended a remote consultation to discuss a referral for psychiatric support to help manage anxiety and depression associated with a hereditary condition. The consultation involved discussion about the possibility of genetic testing.
Following the consultation, the patient expressed dissatisfaction with the manner in which the discussion had been conducted. They felt the conversation was not handled with sufficient sensitivity given the emotional and psychological implications of their family’s genetic history. The patient also reported feeling pressured into considering genetic testing rather than being supported to make an informed and autonomous decision at a pace that suited them.
The patient subsequently submitted a formal complaint, raising concerns about both the consultation and the way their complaint was managed. They felt the complaint process focused primarily on clinical and procedural aspects, without due consideration for the emotional distress caused by the experience. They also felt that appropriate redress was not offered and that their emotional harm had not been acknowledged.
An independent adjudicator reviewed the case. The complaint about the consultation was upheld, and the complaint about complaint handling was partly upheld.
The adjudicator found that while the Stage 2 complaint review was conducted appropriately, the Stage 1 investigation fell short of the standards outlined in the ISCAS Code. A goodwill payment of £350 was awarded to the patient in recognition of the service shortfalls identified.
Learning and Key Takeaways for Healthcare Professionals
This case underlines the importance of sensitive communication, patient-centred care, and robust complaint-handling processes, particularly when consultations involve emotionally charged or ethically complex topics such as genetic testing.
1. Acknowledge and Inform Early
Formally acknowledge complaints as soon as they are received and provide the complainant with a copy of the organisation’s complaint process. Early clarity helps manage expectations and demonstrates transparency.
2. Define the Scope of the Complaint
Agree on the specific issues (or “heads of complaint”) with the complainant before commencing the investigation. This ensures that the response addresses all concerns and avoids misunderstanding.
3. Maintain Comprehensive Records
Document all communications with complainants—including telephone calls and informal conversations. Accurate records support accountability, continuity, and consistency across different stages of the complaint.
4. Apply Empathy and Offer Redress Where Appropriate
Recognise and acknowledge emotional impact, not just procedural or clinical elements. Consider appropriate goodwill gestures that demonstrate empathy and a genuine desire to resolve the matter.
5. Reinforce Staff Awareness of Standards
Use complaint outcomes as learning opportunities. Encourage staff to familiarise themselves with the ISCAS Code and take advantage of training resources such as ISCAS short videos to improve consistency and quality in complaint handling.
Summary
This case illustrates the critical role of sensitivity, empathy, and effective communication in patient interactions, especially when discussions involve genetic or mental health considerations. It also highlights the value of transparent and patient-centred complaint handling as part of maintaining trust and supporting continuous quality improvement.